Microbiota and cancer: The invisible influence on health and disease
The gut microbiota is a complex ecosystem made up of a variety of microorganisms, such as bacteria, viruses, fungi, archaea, and protozoa, that live in symbiosis with the human body. This group of organisms not only facilitates the digestion and absorption of nutrients, but also plays a crucial role in regulating the immune system, producing vitamins and other essential metabolites, and protecting against pathogens that can trigger disease.
When the microbiota is balanced, its functions are highly beneficial for overall health. For example, gut bacteria produce short-chain fatty acids like butyrate, which not only nourish colon cells but also have anti-inflammatory properties. Similarly, this microbial balance contributes to the maturation of the immune system, helping to keep the body's natural defenses active and efficient, and preventing harmful organisms from adhering to the intestinal tract.
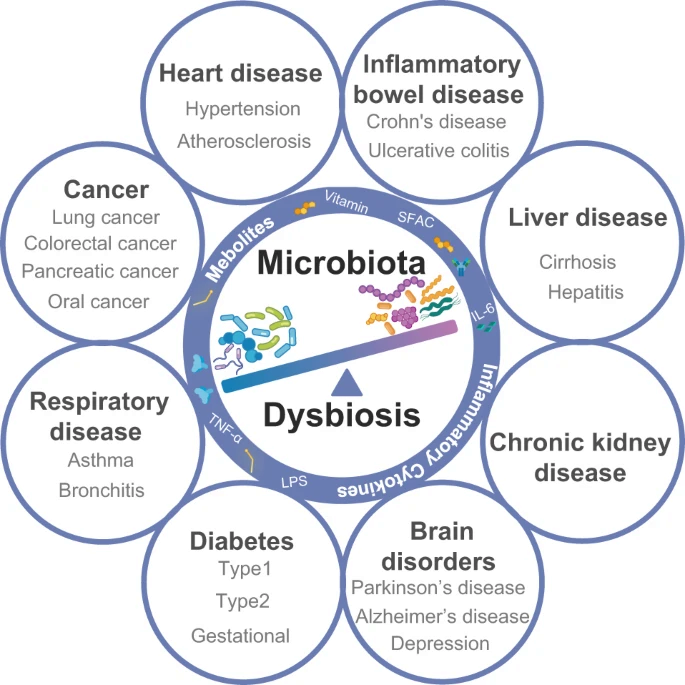
However, when external factors disrupt this balance—such as a diet rich in ultra-processed foods, a sedentary lifestyle, chronic stress, unnecessary antibiotic use, or exposure to environmental pollutants—a phenomenon known as dysbiosis can occur. Dysbiosis describes an imbalance in the composition of the gut microbiota, where certain pathogenic or unbalanced microorganisms proliferate at the expense of beneficial ones. This imbalance is associated with an increase in chronic low-grade inflammation, which in the long term can contribute to the development of chronic diseases such as autoimmune diseases, metabolic problems, digestive disorders, and even cancer.
The link between microbiota, oxidative stress, and chronic inflammation in cancer development
Oxidative stress and chronic inflammation are interrelated factors that play a fundamental role in the development of cancer. These processes not only affect the body's cells but are also strongly modulated by the state of the gut microbiota. An imbalance in the microbial composition can trigger a series of reactions that alter the intestinal environment, increasing the production of reactive oxygen species (ROS), thereby increasing inflammation.
Gut dysbiosis contributes to oxidative stress by disrupting the normal function of immune cells and promoting the release of inflammatory molecules. This chronic, low-grade inflammation, which is often present in conditions such as obesity, insulin resistance, and unhealthy diet and lifestyle, damages cells, tissues, and DNA, creating an environment conducive to tumor development. Furthermore, cumulative cellular damage from oxidative stress can lead to genetic mutations that promote the formation of cancer cells.
Recent studies have shown that certain intestinal microorganisms, such as colibactin-producing Escherichia coli , are capable of inducing DNA breaks, which increases the likelihood of genetic alterations associated with cancer, especially in the gastrointestinal tract. These effects are not limited to the intestine; microbial imbalance also has implications for other organs, such as the liver and lungs, where altered microbiota can contribute to the development of specific cancers.

|
"Oxidative stress and chronic inflammation, modulated by the microbiota, are key factors in the development of cancer." |
Characteristics of the microbiota in people with cancer
The gut microbiota of people with cancer displays distinctive patterns that can influence both the development and progression of the disease. An imbalance in microbial composition has been shown to be associated with several types of cancer, including colorectal, breast, liver, and lung cancer. Altering the microbiota can modify the body's immune response, allowing tumor cells to evade attack by the immune system, a crucial factor in cancer progression.
In people with cancer, there is a reduction in microbial diversity, a key marker of dysbiosis, and an overabundance of certain pathogenic bacteria, such as Fusobacterium nucleatum in colorectal cancer. This bacterium has been linked to the induction of chronic inflammation and altered immune responses, factors that promote tumor progression. Furthermore, some bacterial species can produce metabolites that affect immune cell function and modify the tumor microenvironment, creating an environment conducive to cancer cell growth.
On the other hand, in many types of cancer, people show a decrease in beneficial bacteria, such as Bifidobacterium and Lactobacillus , which have anti-inflammatory and immune-modulating properties. This decrease may contribute to a state of chronic inflammation, promoting carcinogenesis. In breast cancer, for example, studies have identified a correlation between altered gut microbiota and an increase in the expression of certain genes associated with cell proliferation, which can enhance tumor formation.
Relationship between microbiota and the effectiveness of cancer treatments
The relationship between the gut microbiota and the efficacy of cancer treatments has emerged as a highly relevant area of research in modern medicine. Several studies have shown that the composition and diversity of the microbiome can significantly influence patients' response to therapies such as immunotherapy and chemotherapy.
Microbiota and Immunotherapy
Immunotherapy, especially immune checkpoint inhibitors, has revolutionized the treatment of several types of cancer. However, the effectiveness of this therapy varies among patients. Research has shown that a diverse and balanced gut microbiota is associated with better responses to immunotherapy. For example, a study published by the U.S. National Cancer Institute found that patients with an abundance of beneficial bacteria were more likely to respond positively to checkpoint inhibitors. In contrast, those with lower microbial diversity showed less favorable responses.
|
"The gut microbiota of people with cancer shows distinctive patterns, such as a reduction in microbial diversity and an overabundance of pathogenic bacteria." |
Furthermore, specific bacteria have been shown to enhance the efficacy of immunotherapy. For example, species of the genus Bacteroides , belonging to the phyla Bacteroidetes and Proteobacteria, are associated with greater therapeutic effectiveness and a reduction in inflammatory side effects. Bifidobacterium species (B. breve, B. longum and B. adolescentis) have also been shown to increase the efficacy of anti-PD-L1 treatments. Likewise, bacteria such as Faecalibacterium prausnitzii , Bacteroides thetaiotaomicron , Holdeman filiformis and Dorea formicogenes have been identified in patients who respond favorably to therapies such as nivolumab and pembrolizumab (immunotherapeutic drugs), contributing to the regulation of inflammation and T cell activation.
On the other hand, members of the Ruminococcus family , more specifically the Clostridium genus , stand out for increasing microbial diversity and enhancing the activity of CD8+ T lymphocytes, essential for the destruction of tumor cells. In particular, Akkermansia muciniphila is more abundant in patients who respond to treatments with anti-PD-1 and can restore the immune response in cases affected by antibiotics. Finally, Enterococcus faecium has been shown to improve therapeutic responses in humans and animal models, especially in combination with anti-PD-1 and anti-CTLA-4. These bacteria open new perspectives for optimizing cancer treatments by modulating the intestinal microbiome.
Microbiota and Chemotherapy
Chemotherapy, one of the mainstays of cancer treatment, is also influenced by the gut's microbial composition. The microbiota can affect the pharmacokinetics of chemotherapy agents, altering their absorption, metabolism, and efficacy. One study highlighted that microbial diversity influences whether a tumor grows, triggers inflammation, or develops immune escape or resistance mechanisms, which can directly impact the efficacy of chemotherapy.
|
"The composition and diversity of the microbiome significantly influence patients' response to therapies such as immunotherapy and chemotherapy." |
Keys to boosting the microbiota in cancer prevention and management
Maintaining a healthy microbiota can be a powerful tool in cancer prevention and management. Some key strategies include:
-
Diet based on “real” foods
A diet based on real foods can be a fundamental pillar in cancer prevention and treatment. A diet rich in fruits, vegetables, quality fish and meat, healthy fats, and anti-inflammatory spices like turmeric and ginger can help keep the body in optimal health. These foods, rich in antioxidants, vitamins, and bioactive compounds, regulate metabolic processes, balance hormones, and reduce the risk of cellular damage.
-
Reduction of processing and refining
Avoiding ultra-processed foods and refined sugars is key to preventing metabolic alterations that can promote uncontrolled cell growth. Ultra-processed foods, rich in additives, trans fats, and empty calories, promote insulin resistance and unbalance metabolism. Refined sugars, meanwhile, generate glucose spikes that stimulate excessive insulin release, creating a favorable environment for the growth of tumor cells, which use glucose as an energy source.
-
Consumption of Probiotics and Prebiotics
Maintaining the gut microbiota through probiotics and prebiotics plays a crucial role in overall health and in the context of cancer. Probiotics, found in fermented foods or supplements, provide beneficial bacteria that improve immune function. Prebiotics, found in foods such as garlic, onions, and asparagus, promote the growth of healthy bacteria that produce protective compounds such as short-chain fatty acids. This intestinal balance can support both prevention and response to treatment.
|
"A diet rich in antioxidants, vitamins, and bioactive compounds can regulate metabolic processes, balance hormones, and reduce the risk of cell damage." |
-
Physical Activity
Regular physical activity plays a key role in promoting a diverse and balanced microbiota, which has significant implications for cancer prevention and management. Exercise modulates the gut environment, promoting the growth of beneficial bacteria that produce short-chain fatty acids, such as butyrate, known for its protective properties against tumor development.
Furthermore, exercise helps reduce systemic inflammation, improves immune system function, and regulates metabolism—key factors in the relationship between microbiota and cancer. Studies show that active people tend to have a more resilient microbiome, which can optimize the response to cancer treatments and improve quality of life.
-
Stress Management
Stress management is equally important, as chronic stress can alter the immune response and weaken the body's defenses. Practices such as meditation, yoga, and mindfulness are effective tools for reducing stress and improving emotional and physical health. These activities not only calm the mind but also positively impact the balance of the nervous system and metabolism. Even something as simple as spending time in nature can improve health markers related to overall well-being.
Conclusion
The gut microbiota plays a central role in health and disease, including cancer. Poor dietary and lifestyle habits can lead to chronic low-grade inflammation, oxidative stress, and unbalance this ecosystem, promoting the development of tumors. During cancer treatment, caring for the gut microbiota is also essential to minimize side effects and optimize clinical outcomes.
Adopting a healthy diet, reducing stress, and adopting beneficial habits are essential steps to maintaining a balanced microbiome, making it a powerful ally in the fight against cancer.
If you'd like to improve your cancer prevention habits, please fill out this form or contact us on WhatsApp here to learn how our team can help.
FOUNTAIN:
Reuter, S., Gupta, SC, Chaturvedi, MM, & Aggarwal, BB Oxidative stress, Inflammation, and cancer: how are they linked? https://pubmed.ncbi.nlm.nih.gov/20840865/
Kandalai, S., Li, H., Zhang, N., Peng, H., Zheng, Q., et al. The human microbiome and cancer: a diagnostic and therapeutic perspective . https://pubmed.ncbi.nlm.nih.gov/37498047/
Sun, Y., Wang, X., Li, L., Zhong, C., Zhang, Y., Yang, X., & Li, M. The role of gut microbiota in intestinal disease: from an oxidative stress perspective . https://pmc.ncbi.nlm.nih.gov/articles/PMC10899708/
Śliżewska, K., Markowiak-Kopeć, P., & Śliżewska, W. (2024). The Role of Probiotics in Cancer Prevention . https://pmc.ncbi.nlm.nih.gov/articles/PMC7793079/
Redalyc. Microbiota, cancer and immunotherapy. https://www.redalyc.org/journal/4577/457763760007/html/
National Cancer Institute. (2018). Gut bacteria as checkpoint inhibitors in the immune response . https://www.cancer.gov/espanol/cancer/tratamiento/tipos/inmunoterapia/inhibidores-de-puntos-de-checkpoint
